Efficient, Compliant, and Revenue-Focused Pharmacy Billing Solutions
Our Pharmacy Billing Services are designed to help independent and specialty pharmacies manage complex insurance claims with accuracy and efficiency. We handle the full pharmacy billing cycle, ensuring timely reimbursements, reduced claim rejections, and strict compliance with payer and regulatory requirements. With our expertise, pharmacies can focus on patient care while we manage the billing process.
- End-to-end pharmacy insurance claim processing
- Accurate NDC and CPT code management
- Eligibility verification and formulary checks
- Prior authorization support
- Rejection and denial management
- Payment posting and reconciliation
- Compliance with pharmacy billing regulations
- Secure, HIPAA-compliant data handling
Online simple step for appointment
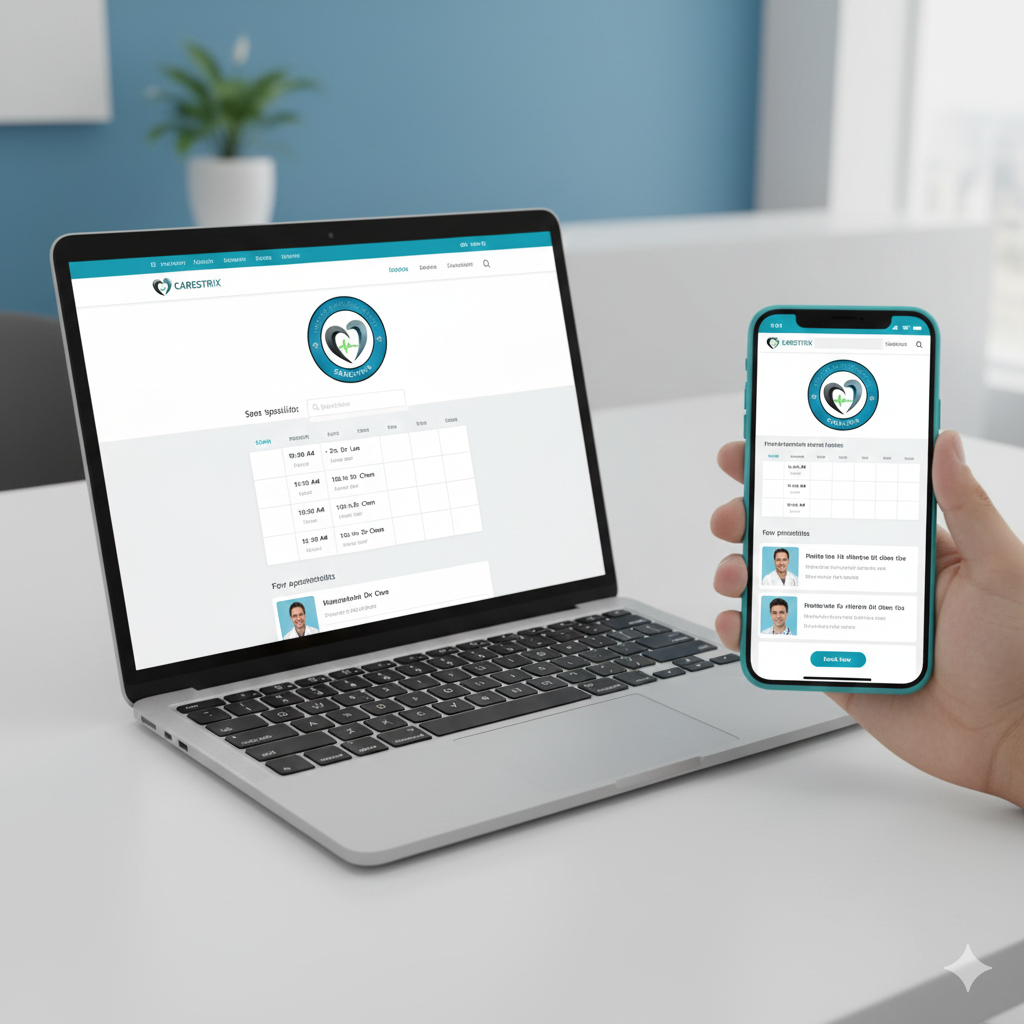
Book Your Free Assessment

Billing Review & Consultation

Start Billing with CareStrix
Frequently asked questions
We support independent pharmacies, specialty pharmacies, long-term care pharmacies, and mail-order pharmacies.
Yes, we assist with prior authorizations to ensure prescriptions are approved and reimbursed without delays.
We focus on accurate coding, eligibility checks, formulary validation, and proactive follow-ups to minimize rejections.
Absolutely. All our pharmacy billing processes strictly adhere to HIPAA compliance standards.
Yes, we provide clear and detailed reports to help pharmacies track claim status, payments, and revenue performance.




